In this article:
-Managing seasonal allergies
-How to prevent joint pain during allergy season
-Food Allergies and joint pain
Do seasonal allergies wreak havoc on your body?
If so, you’re not alone — many people experience an increase in their allergy symptoms during allergy season, especially when pollen counts are high. For some, symptoms are mild, with sneezing and stuffiness, while others experience joint, back and neck pain, in addition to breathing difficulties. However, although allergies can cause neck pain, join pain and back pain, there are many things you can try to make the pain subside.
In some cases, your symptoms may appear to be related more to the weather, injury or illness rather than specific allergens. However some allergy symptoms, such as non-allergic rhinitis and even joint pain, can be brought on by rapid changes in temperature and humidity that typically accompany the spring season. In the United States, spring often is the highest time for allergies, meaning your seasonal allergies could be the cause of your pain.
Let’s take a closer look at how allergies and joint pain may be related.
What Causes Back Pain?
Back pain is a common complaint, especially among adults. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, there are several potential causes of back pain.
Aging is one of the most common risk factors, as people may begin to experience back pain between the ages of 30 and 40. It is also a more prevalent issue among those who are not physically fit. Another risk factor is being overweight, which stresses the back and leads to pain. There are also hereditary factors, such as ankylosing spondylitis, a form of arthritis that can impact the spine. Back pain may also be caused by diseases such as cancer and arthritis.
Pain in the lower back is particularly common and is one of the leading reasons for people to go to the doctor or to stay home from work. Back pain can occur in acute or chronic forms. Acute pain is pain that begins suddenly and that typically lasts for six weeks or less. Chronic pain is more prolonged, such as pain lasting longer than three months. Chronic pain is less common than acute pain. It is possible for acute back pain to improve without treatment, depending on the underlying cause. You may find that taking ibuprofen, acetaminophen or aspirin can help to reduce your back pain.
There are several potential causes of back pain, including specific problems related to certain conditions or diseases:
- Arthritis
- Spinal stenosis
- Infections
- Kidney stones
- Scoliosis
- Muscle spasms
- Disk breakdown
- Ruptured disks
- Tense muscles
- Seasonal allergies
You may have more than one underlying cause linked to your back pain. If you have strong symptoms and aren’t feeling well, you’ll want to consider treatment options with your healthcare provider.
How Can You Treat Back Pain?
If you’re suffering from back pain, there are several potential treatments to consider.
Medications, like topical analgesic creams and ointments, may offer pain relief. Analgesic medications are over-the-counter medications, such as aspirin or acetaminophen. Nonsteroidal anti-inflammatory medications can reduce pain and swelling. These drugs often referred to as NSAIDs, include common over-the-counter medications such as ibuprofen and naproxen sodium. It is possible to get a stronger NSAID from a doctor.
If you have chronic back pain, additional medications may include muscle relaxants and even antidepressants. However, these options may not work for everyone.
Medications are just one treatment option. You may prefer to use hot or cold packs, or both, to ease a sore and stiff back. These packs offer a number of benefits. Heat helps reduce pain and muscle spasms, while cold reduces swelling and numbs more intense pain.
Exercise is another treatment option, especially if the cause of the problem is weight-related. However, it is important to note that while exercise can ease chronic pain, it is not ideal for acute back pain. Individuals suffering from either types of pain should seek advice and clarification from a doctor or physical therapist.
Joint Pain: You’re Not Alone

In a recent national survey, nearly one out of every three adults in the US reported having joint pain within the last 30 days. In this survey, deep pain was the most common complaint, followed by shoulder and hip pain
Joints connect your bones together, providing your body with support as you move. Joint pain can impact just about any part of your body, including the ankles, feet and hands. While joint pain can occur at any age, it becomes increasingly common as a person ages.
Damage to your joints caused by injury or disease cannot only interfere with movement, but can also be a common cause of pain. Some of the most common conditions leading to painful joints include rheumatoid arthritis, bursitis, osteoarthritis, gout, strains, sprains and other injuries, such as in sports.
As with back pain, joint pain can vary greatly in terms of severity in the amount of time that it lasts. For example, joint pain that resolves within a few weeks is referred to as acute. However, many people suffer from chronic joint pain, or pain that lingers for weeks or months at a time.
Other common causes of joint pain include:
- Osteoarthritis
- Tendinitis
- Overuse injuries, such as strains are sprains
- Gout
- Certain injuries, such as a fracture
- Infections caused by a virus
- Bursitis
- Autoimmune diseases, including lupus and rheumatoid arthritis
- Seasonal allergies
Can Joint Pain Be Treated?
To help understand joint pain, your doctor will first try to determine an underlying cause. Once you discuss the potential causes with your doctor, treatment options can vary based on the reason for the joint pain.
As with back pain, over-the-counter anti-inflammatory medication such as aspirin or ibuprofen may help with moderate to severe joint pain. If you have milder pain that is not accompanied by inflammation, it is possible that taking Tylenol for a short period of time will provide relief.
Other drugs that may help reduce joint pain include antidepressants, antiepileptic drugs and muscle relaxants that can treat muscle spasms. Some people may find relief by taking two drugs at once, such as muscle relaxants and NSAIDs. It is important to consult with a doctor before doing this.
Seasonal Allergies: Occurrence and Symptoms
Seasonal allergies are sometimes referred to as hay fever or allergic rhinitis.
In the United States, allergies typically are at their worst during the spring season, when flowers start to bud and trees begin to bloom. In most parts of the country, allergies typically start in February and can last until early in the summer.
Certain factors can influence the intensity and duration of allergy season. For example, milder winter temperatures can lead to early plant pollination. Additionally, a rainy spring can lead to rapid plant growth, ultimately causing an increase in mold and symptoms that can linger into the fall.
Seasonal allergies develop because the body’s immune system has become sensitized and is overreacting to something in the environment that normally does not cause problems in other people. Some of the most common triggers of seasonal allergies include grass, pollen and mold.
Some of the most common general allergy symptoms include:
- Nasal congestion
- Coughing
- Sneezing
- Wheezing
- Runny nose
- Itchy throat
- Itchy skin
- Itchy and watery eyes
- Hives
- Fatigue
- Joint, back and neck pain
Other factors can influence the severity of allergy symptoms. After a rainfall, pollen counts typically increase. Pollen counts are often higher on warm and windy days. On days with no wind, allergens are typically grounded. High humidity also promotes mold growth. In addition, pollen levels are generally at their highest in morning hours. Certain pollens, such as grass and ragweed, are most prevalent when the nights are cool and the days are warm.
Managing Your Seasonal Allergies

One of the most important things someone suffering from allergies can do is to identify the triggers. While some people seem to blame one trigger, it is possible that there are actually multiple triggers. It is not uncommon for those who suffer from spring allergies to show symptoms throughout the year. Some ways to avoid triggers include:
- Shower after being outdoors.
- Monitor pollen and mold counts, which are available on TV or in the news.
- Stay inside during peak pollen counts, which is the middle of the day of the afternoon.
- Wear a filter mask when working outdoors.
- Take preventive medication.
You can take other precautions as well, such as bathing and shampooing your hair each day to completely remove the pollen from your hair and skin. You should also wash your bedding in hot soapy water at least once a week.
You may need to wear sunglasses outdoors to protect your eyes from pollen. Those with severe allergies might find that a facemask is helpful during times when daily pollen counts are very high. It is also important to avoid line drying your bedding or clothes outdoors if the local pollen counts are high, as pollen can settle on these items.
Treatment options may include one or more medications to help control symptoms. While some drugs are available over-the-counter, others may require a prescription. Common medications to treat allergies include nose sprays and anti-histamines. Many people find that allergy shots provide relief, especially if their symptoms are linked to pollen. Allergy shots work by exposing the body to small amounts of allergens, which gives the body time to learn how to tolerate the allergens.
Can Seasonal Allergies Cause Body Aches, Back Aches and Joint Pain?
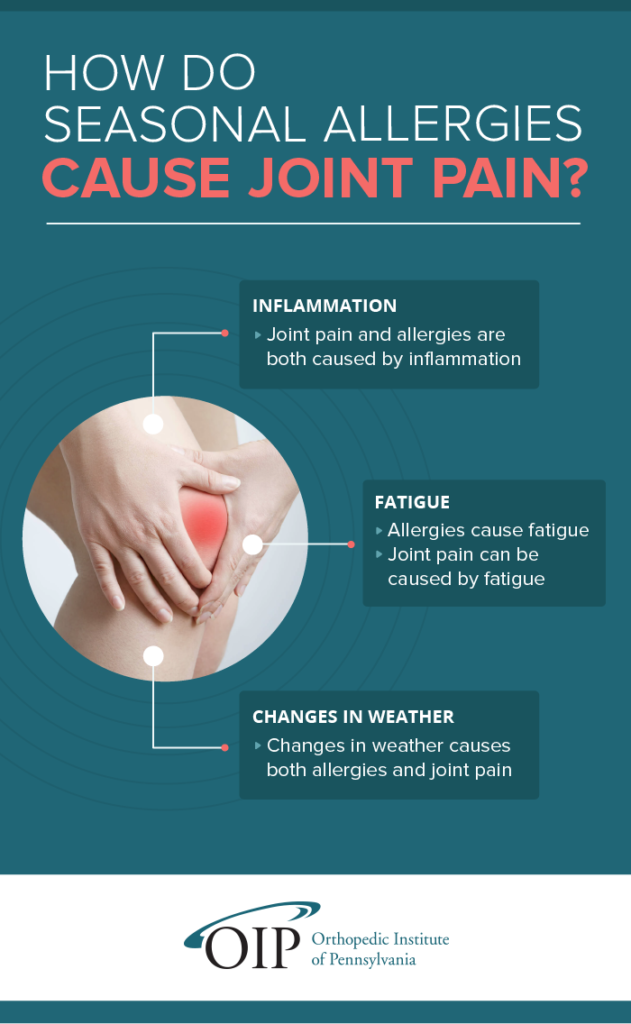
If you’re wondering whether seasonal allergies can cause back aches and joint pain, you’re not alone. There are plenty of ways seasonal allergies are related to back pain and joint pain as well.
For starters, it is possible to experience joint pain with a cold. Because both allergies and a cold cause similar symptoms, such as a runny nose and sneezing, itchy eyes and throat, and stuffy nose, some people confuse a cold with allergies.
Colds are typically accompanied by a sore throat and coughing, and maybe even a fever and body aches in your neck. However, some people who suffer from inflammation because of their allergies experience joint pain as the body attempts to flush out the allergen.
Can seasonal allergies cause joint inflammation?
Another potential link is that allergies can lead to fatigue, which can also make sore joints feel worse. Changes in weather can also lead to joint pain. This is especially true for cold and damp climates and weather-related changes that coincide with seasonal allergies.
Muscle and joint pain can be a coexisting problem resulting from arthritis, Lyme disease and certain immune disorders. It can also be linked to bursitis and osteoporosis. There are other potential causes as well.
If you experience sneezing and coughing as a result of your allergies, you may suffer from muscle, joint and neck pain due to the repeated sneezing or coughing. Seasonal allergies can also make you feel tired, which can ultimately make your symptoms worse.
If you’re not sure whether your joint pain is caused by allergies, the best way to distinguish symptoms is to take a short course of antihistamines. You can take antihistamines for a week to determine whether allergies may be a source for your pain.
How to Prevent Joint Pain During Allergy Season
There are many possible treatment options for allergies, which can keep joint and back pain at bay.
For airborne allergens, you might find relief through humidifiers, air purifiers, filters and conditioners. In addition, many people find that over-the-counter medications, prescription medications or a combination of both also offer relief.
Antihistamines are medications that help counterbalance the effects of histamine, the common substance in allergens that leads to allergy symptoms. Immunotherapy through allergy shots and anti-inflammatory nasal steroid sprays are another treatment option. These sprays work by reducing swelling and inflammation, which cuts down on mucus production. Nasal steroids work especially well when combined with antihistamines.
Decongestants, available in capsule form, help to reduce sinus swelling and discomfort by thinning nasal secretions. These medications are intended for short-term use and are often combined with antihistamines for full relief from symptoms.
Seasonal Allergies and Joint Inflammation
If joint pain occurs during allergy season, you can experiment with a variety of treatment options to find what works best for your joint pain. Over-the-counter medications such as Tylenol and Advil can work for mild pain. For acute pain, hot or cold packs might provide relief. Your doctor might recommend steroid shots, where medication directly into the joint to help reduce pain and inflammation.
Some individuals also find that physical therapy can help to strengthen muscles around the joint, which in turn strengthens the joint and improves the range of motion.
Food Allergies and Joint Pain & Inflammation
Seasonal allergies aren’t the only type of allergies that can contribute to joint pain. There are also certain pre-existing conditions and food allergies that can cause joint inflammation and your body to have inflammatory responses. Inflammation is what causes the joints to swell and create pain or discomfort. There are two main culprits for food-related joint pain:
- Arthritis
- Food allergy or sensitivity
If you already have arthritis, then you probably have experienced some amount of joint pain in the past. Although there are many different types, arthritis is basically inflammation that affects your joints, causing pain and stiffness. Some patients with this condition experience increased inflammation after eating certain foods. This is especially true of patients with rheumatoid arthritis, an autoimmune disease that causes chronic joint inflammation, especially in the hands and feet.
Even though arthritis causes your body to be in a constant inflammatory state, it’s important to be aware of the triggers that can cause bouts of increased inflammation and lead to painful joint symptoms. Some foods known to impact arthritic patients and cause joint pain include:
- Sugar: Releases inflammatory messengers called cytokines.
- Saturated Fats: This triggers fat tissue inflammation. Foods to watch out for are pizza, cheese, red meat, pasta dishes and grain-based desserts.
- Trans Fat: This is commonly found in fast food and processed foods like snacks, cookies, crackers, doughnuts and even margarine. Trans fat can trigger systemic inflammation.
- Omega 6 Fatty Acids: Although omega 6 fatty acids are essential to a healthy diet, arthritic patients should watch how much they ingest as it can produce pro-inflammatory chemicals. Omega 6 is found in mayonnaise, salad dressing and a variety of oils like corn, peanut, grapeseed, soy, sunflower and more.
- Refined Carbs: Products with white flour, white rice and white potatoes can fuel the production of advanced glycation end, which increases inflammation.
- MSG: Often found in prepared Asian food and other types of prepared foods, this chemical is a known trigger for chronic inflammation.
- Alcohol: Although alcohol most notably impacts liver health, it can also cause inflammation when not used in moderation.
If you don’t have arthritis, you may find that you experience pain in your joints after you eat certain meals. Foods can still cause joint pain if you have a food allergy or a sensitivity to particular ingredients. When you experience joint pain with no specific cause, then it may be time to take a closer look at your diet. There are a number of different tests a specialist can use to determine your own personal food and drink intolerances, such as:
- Food allergy/sensitivity test
- Stool analysis
- Elimination diet
- Nutritional deficiency test
Whether it be gluten, dairy or an assortment of other foods, identifying and eliminating these triggers from your diet could help you manage joint pain. An anti-inflammatory menu will also be beneficial to your overall health and well-being.
What if Your Pain Continues?
Despite your best efforts, you may find that your chronic pain does not resolve over time. This is especially true if you have already tried a combination of pain relief methods and treatment for allergies.
Your pain might be more than allergies. To be sure, schedule an appointment at one of OIP’s designated care centers today. We’re here to help!