OIP Safe Summer Fun Series: Golf

OIP Safe Summer Fun Series: Golf
- Golfer’s elbow, technically called medial epicondylitis, happens when the forearm muscles that connect to the elbow bone become aggravated and sore. Some year-round exercises that can help include squeezing a tennis ball as well as doing wrist curls/reverse wrist curls. Wrist curls are performed by placing a light weight (dumbbell) at your fingertips and rolling it back to the palm. You can also raise your wrist to elevate the weight by an inch or so and do the exercises again. Alternate arms and do 10 of these rolls in a set. Reverse wrist curls are done by placing a light weight on the back of the hand while having it extended in front of you. Raise and lower the weight using only the forearm. Brace your arm with the other arm to help limit your motion. These can also be done in sets of 10.
- Low back pain is many times the result of improper form, decreased strength, or due to a lack of flexibility. Some activities that can help include rowing, pull-downs, and yoga/pilates. To perform some basic rowing and pull-down activities, securely tie some rubber tubing and place it around a shoulder-height object, such as the hinge of a door. Keeping arms extended in front of you, slowly pull the tubing toward your chest and then slowly release. You can also kneel and pull the tubing down to your chest slowly and return it slowly. Be sure to bend the elbows as you pull. Three sets of 10, three times per week will get you off to a great start.
- Other things to keep in mind are to do some warm-up exercises, stretch, and hit a few balls on the driving range before heading out to the course.
- Wear sunscreen, avoid golfing during storms, stay hydrated, and always follow proper cart safety.
- Be vigilant of the activity of other golfers; you can be injured by a wayward golf ball.
Safe Summer Fun Series: Swimming

- Make sure you know how to swim, and never swim by yourself. Have life jackets available for those with less experience. When at the beach or other large swimming areas, be sure to stay within the patrolled areas under a lifeguard’s watch.
- Only swim if you are healthy enough to do so; check with your doctors if you have any questions.
- Be sure to warm up with some land-based exercises, and remember to stretch!
- Shoulder injuries are at the top of the list, so exercising-and thereby strengthening-shoulder and upper back muscles will help.
- Never go into a body of water head-first, and never dive into shallow or murky water.
- Make sure the area is deep enough for diving, and always enforce proper diving board use. Be sure that people do not dive until the last diver is out of the way.
- Check the weather! Thunderstorms-and therefore electrical activity-and water are not a good mix. Wait it out inside the house if a storm is on its way.
- Never enter lakes or large bodies of water after a storm if there appears to be any flooding or murky water. Hazards can arise after storms.
- Enforce a “no drinking and swimming” rule. Alcohol impairs judgment, movement, and vision, and it can also make it difficult for a person to maintain proper body temperature.
- Be prepared for bumps, scrapes, and other minor injuries with basic first aid supplies, and always have a way to reach emergency personnel if needed.
Have fun and be safe!
AAOS. “Swimming Injury Prevention.” OrthoInfo. American Academy of Orthopaedic Surgeons. 1995-2017. Web. July 2017.
OIP Safe Summer Fun Series: Trampolines

• Regularly inspect the unit and make repairs promptly.
• Make sure there is adult supervision/spotting taking place during use.
• Children under six years of age should not use trampolines.
• Allow only one jumper at a time.
• Do not allow high-risk behavior such as flips.
• Take ladders away when the trampoline is not in use; this prevents youngsters from climbing in unsupervised.
• Bounce houses, while different in structure, are similar in risks and recommendations.
Have fun and be safe!
-Your friends at OIP
AAOS. “Trampoline Injury Prevention.” OrthoInfo. American Academy of Orthopaedic Surgeons. 1995-2017. Web. July 2017.
Attention patients with United Health Care insurance!
Important Notice:
You may have recently received a letter stating that Pinnacle Health and OIP will no longer be participating with your insurance plan starting June 1, 2017. This is incorrect. OIP will remain a participating provider with your insurance. If you have concerns about coverage of services within Pinnacle Health system, please contact the member services number on the back of your insurance card to inquire. Please contact our billing office at (717) 761-5530 for additional information. Thank you.
Make May Count
- Make May the month you schedule a DEXA, or bone density, exam.
- Make May the month you start calcium and Vit D supplementation.
- Make May the month you start some weight-bearing exercises.
- Make May the month you ask your family doctor or OIP provider about osteoporosis.
- Make May count

We’re never too old to get in shape!
Robert Marchand is a 105 year old cyclist who had improved his world record for how far he could ride a bicycle in one hour from 15.1 miles at age 101 to 16.7 miles at age 103. That is an 11% improvement in performance due to vigorous training. Impressive at any age!
In addition, his blood tests that are used as markers of aging improved over those two years!
His program? One day a week, intensive long duration cycling (at least 3 hours long) to deplete his muscle sugars. This allowed him to store more energy in his muscles for future workouts.

Two days a week, he did intensive interval training that involved exercising as hard as he could for 30 seconds to two minutes multiple times until fatigue.
The remaining 4 days a week, he did relaxed bike rides in order to recover from the other intense workouts. He exercised every day of the week.
So, Robert Marchand proves that you are never too old! Get out there and exercise!
Video
The Orthopedic Institute of Pennsylvania Welcomes New CEO

The largest provider of orthopedic care in the South Central PA region has successfully recruited a new CEO to take over the reins starting in April.
William C. Thompson, II is leaving his position as the Director at the world-renown Hedley Orthopedic Institute in Phoenix, Arizona to join OIP. Prior to his work in Phoenix, he was the Director of Operations at the Cardinal Orthopedic Institute in Columbus, Ohio. He also has significant experience as a high level administrator in the acute care hospital setting and in urgent care.
Will earned a BA from the Ohio State University in Political Science and an MBA at OSU’s Fisher College of Business.
He is replacing Dr. Jack Frankeny who is retiring from clinical practice and administration.
The Orthopedic Institute of PA sees patients in 14 locations in Cumberland, Dauphin, Perry, Northumberland, Fulton, and Huntington Counties. They employ nearly 300 employees.
Lyme Disease & Joint Pain
-Symptoms of Lyme Disease
-Treatment of Lyme Disease
-Prevention of Lyme Disease
If you are wondering if a disease can cause all your joints to hurt, Lyme disease is most likely the answer. An infection caused by bacterium carried by deer ticks, Lyme disease can be effectively treated with antibiotics when caught early. However, when undiagnosed and left untreated, the infection can potentially spread to your nervous system, heart and joints, resulting in a complex and debilitating disorder that is more difficult to treat.
Can Lyme disease cause joint pain? The simple answer is yes it can. Here we’ll provide more information on Lyme disease and its relationship to joint pain.
How Do You Get Lyme Disease?
In the U.S., Lyme disease is carried primarily by deer or blacklegged ticks, and it is caused by the Borrelia mayonii and Borrelia burgdorferi bacteria. It’s easy to be bitten by ticks in high-risk areas such as Central PA. The creatures are often no bigger than a poppy seed, so they are very difficult to see before they latch on.
However, not all ticks are Lyme disease carriers. To contract the disease, an infected tick needs to bite you. Bacteria from the tick will eventually make its way from the bite through to your bloodstream, usually taking between 36 to 48 hours. For this reason, whenever you’ve been in the outdoors, particularly in a known tick-heavy area, you should always check your body for parasites before you come back inside.
In the two primary stages of life, U.S. deer ticks feed on rodents, which are a prime source of the bacteria that causes Lyme disease. Ticks move onto feeding primarily on white-tailed deer when they reach adulthood.
If you find a swollen tick attached to you, it could have fed for long enough to transmit bacteria and should be removed with tick tweezers as soon as possible to prevent infection.
Risk Factors for Acquiring Lyme Disease
Where you vacation or live, as well as what outdoor activities you participate in, affects your likelihood of being exposed to Lyme disease. Common factors that put you at risk of contracting Lyme disease include:
- Spending time in grassy or wooded areas. Deer ticks are very prevalent in the Central PA area due to its heavily wooded countryside. Deer ticks thrive in these types of places. Children here are particularly at risk as well as adults who work outdoors.
- Having exposed skin. Ticks find it easy to attach themselves to exposed skin, so if you’re in an area that’s known for ticks, always wear long sleeves and long pants and never allow your pets to run through long grasses.
- Removing ticks incorrectly or not quickly enough. As you already know, bacteria from a tick bite has the potential to enter your bloodstream if the tick has been attached to you for between 36 to 48 hours or longer. If you spot and correctly remove the tick within 48 hours, your risk of acquiring Lyme disease is low, so always check your skin after being outdoors.

The Centers for Disease Control and Prevention notes that older adults and children are most susceptible to the disease, along with others, like park rangers and firefighters, who spend time outside. It’s estimated that 300,000 people nationwide are diagnosed with Lyme disease each year.
Facts About Lyme Disease in PA

Ticks thrive in the countryside of Pennsylvania in particular, and according to a study published in the Proceeding of the National Academy of Sciences of the United States of America (PNAS), Lyme has a greater likelihood of occurring where suburban developments encroach on existing forest. This is thought to be because the white-footed mouse that is the most important animal in the Lyme disease transmission cycle can live without too many predators under these circumstances.
Notable statistics of Lyme disease in PA include:
- Pennsylvania ranks at number one in terms of Lyme disease cases across the US.
- Pennsylvania reported 7,400 new cases of Lyme disease in 2014 alone. This was a 25 percent increase on the previous year’s numbers, and experts believe that the actual number could be as many as 10-12 times higher.
- Pennsylvania contains 67 counties, and all have reported cases of Lyme disease.
- Pennsylvania contains a reported 10 tick-borne diseases.
What Are the Common Symptoms of Lyme disease?
In the early stages of infection, symptoms of Lyme disease are very similar to a mild flu, including
- Headache
- Fever
- Chills
- Fatigue
- Swollen lymph nodes
For some people, a telltale sign of the disease is the red bull’s eye-shaped skin rash that presents in some, but not all sufferers, within three to 30 days after being bitten by a tick.
Often, these first signs are missed when you’re infected with Lyme disease and are dismissed as the flu or some other virus. This is very worrying because if antibiotic treatment isn’t begun when the first signs of the disease present, your condition can become more serious.
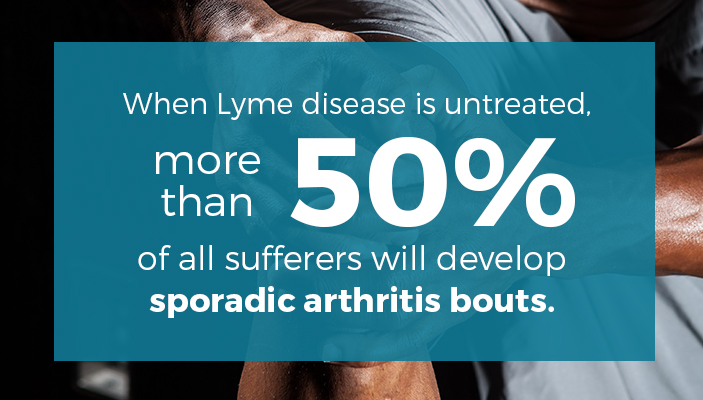
Joint pain is another issue that can occur with Lyme disease. In the worst cases, over several weeks, nervous system and heart issues can develop. If left untreated, you may suffer from arthritis and neurological issues. In fact, according to the Arthritis Foundation, when Lyme disease is untreated, more than half of all sufferers will develop sporadic arthritis bouts.
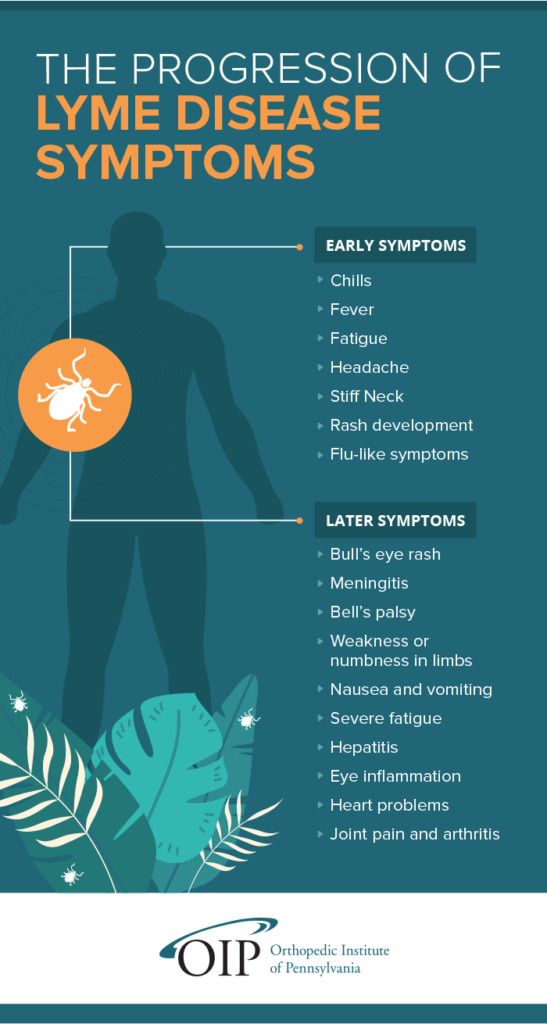
Although the symptoms and signs of Lyme disease can vary from person to person, they generally appear in stages with early symptoms and signs appearing first, followed by later ones.
Early Symptoms and Signs of Lyme Disease
You can expect a small, red bump on the site of your bite, or where you removed the tick from, and this will resolve within a day or two. This is to be expected after being bitten by any insect, and it in itself is not an indicator that you have Lyme disease.
However, if you have been infected, you can expect the following within a month or so:
- Flu-like symptoms. Early-stage Lyme disease can present as chills, fever, fatigue body aches, stiff neck, headache and other flu-like symptoms.
- Rash development. Between three and 30 days after an infected tick bites you, you may see a rash that looks like a bull’s eye. This will expand over days, and it can grow to as many as 11 to 12 inches across. It is usually not painful or itchy.
Later Symptoms and Signs of Lyme Disease
If you don’t seek treatment, other symptoms and signs of infection may appear over the following weeks and months, including:
- The bull’s eye rash. It is also called erythema migrans, and it may appear on other areas of your body.
- Neurological problems. At any time after the initial Lyme disease infection, even years later, you could develop meningitis, Bell’s palsy (temporary paralysis of one side of your face), weakness or numbness in your limbs and impaired muscle movement.
You may also suffer from:
- Other rashes
- Nausea and vomiting
Many weeks after infection, some people develop:
- Severe fatigue
- Hepatitis
- Eye inflammation
- Heart problems that last either for days or weeks
- Joint pain and arthritis
The Progression of Lyme Disease
Lyme Disease, Joint Pain and Arthritis
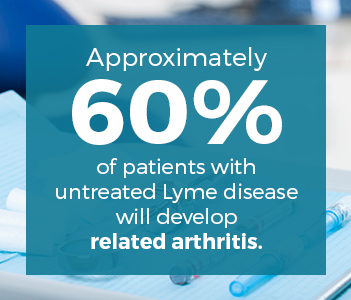
Lyme disease and joint pain unfortunately go hand in hand, as Lyme-related arthritis is commonly found in Lyme disease sufferers. If you have Lyme arthritis, you have swollen, painful and aching joints that cause stiffness and pain. It is found in people who are in the late stages of Lyme disease. According to an article in Science Daily, approximately 60 percent of patients with untreated Lyme disease will develop related arthritis.
Lyme arthritis is caused by the bacteria that causes Lyme disease getting into your joints and causing inflammation of your tissues. Over time, this can cause damage to your cartilage. Most cases of Lyme arthritis are short-lasting and affect only one large joint.
Lyme arthritis can affect your:
- Knees (most common)
- Wrists
- Ankles
- Hips
- Elbows
- Shoulders
In the U.S., it’s estimated that about 60 percent of untreated Lyme disease patients will experience intermittent episodes of swelling and lyme disease joint pain for months to years after they are infected by a tick bite.
Thankfully, most Lyme arthritis cases can be treated with antibiotics and NSAIDs, although some people may require surgery to remove some diseased tissue. Around ten percent of untreated patients may go on to develop chronic arthritis, reports Johns Hopkins Arthritis Center.
How Is Lyme Disease Diagnosed?
As the symptoms and signs of Lyme disease are similar to those found in other conditions and are nonspecific, diagnosis is not easy. In addition to this, the ticks that spread the disease can also transmit other diseases at the same time.
Diagnosis is easier when your doctor can see that you have the characteristic bull’s eye rash. However, if you don’t, your doctor will ask you about your medical history, whether you’ve been outdoors in summertime, where you have been outdoors and will give you a medical examination.
Lab tests enable bacteria antibodies to be detected in order to confirm a diagnosis. They are most reliable when you’ve had the infection for a few weeks, as your body will then have had the time to develop the antibodies.
Tests for Lyme disease include:
- Enzyme-linked immunosorbent assay (ELISA) test. This is the test most commonly used to diagnose Lyme disease, and it detects antibodies to Borrelia burgdorferi bacteria. Sometimes the test brings up a false-positive so it’s not typically used as the sole test for diagnosis.
Although the test may not show as a positive result during the first stage of Lyme disease, often the accompanying rash is distinctive enough to make the diagnosis, especially if you’ve been in an area where Lyme disease-transmitting ticks are common.
- Western blot test. If the initial ELISA test comes back positive, the Western blot test will confirm your diagnosis.
How Is Lyme Disease Treated?
Generally speaking, the earlier and more quickly Lyme disease is treated, the quicker and more complete your recovery will be.
Antibiotics are used to treat Lyme disease, and they include:
- Oral antibiotics. Oral antibiotics are the standard treatment for Lyme disease when it’s in its early stages. Cefuroxime or amoxicillin is prescribed for younger children, breastfeeding or pregnant women and some adults. Doxycycline is given to children and adults over the age of eight years.
The usual length of a course of antibiotics for Lyme disease is between 14 and 21 days.
- Intravenous antibiotics. If you are suffering from complications affecting your central nervous system, you may be prescribed treatment via intravenous antibiotics for between 14 and 28 days. This course of action gets rid of any infection, although it may still take you a long time to recover entirely from your symptoms.
Intravenous antibiotic treatment often causes a range of side effects, including:
- Mild to severe diarrhea
- Lower white blood cell count
- Infection or colonization with other antibiotic-resistant organisms
Even though there is a risk of experiencing these side effects, it’s imperative to undergo the course of treatment your doctor prescribes to avoid the serious complications Lyme disease can have.
It’s important to remember that even after you’ve finished your treatment, you may still experience other symptoms, like fatigue and muscle aches. This is known as post-treatment Lyme disease syndrome, and the cause of the condition is as yet unknown.
Treating Lyme Disease-Related Joint Pain
When a patient with Lyme disease presents with joint pain symptoms, they may be suffering from Lyme arthritis. If antibiotics are not used to treat Lyme disease, there’s a good chance that a patient could develop Lyme arthritis. For most people, once the underlying bacterial infection is treated, the associated arthritis also resolves with no additional treatment required.
However, in some cases, even when the Lyme disease is treated with oral or intravenous antibiotics, the arthritis persists. This is known as antibiotic-refractory Lyme arthritis, which means patients may need medications that treat the pain and inflammation associated with arthritis. The main way that doctors determine if a patient has arthritis despite being treated for Lyme disease is the persistent inflammation that causes joint pain.
It’s believed that patients with antibiotic-refractory Lyme arthritis are more susceptible to excessive inflammation due to two factors:
- A bacterial strain that is particularly inflammatory
- Patient genetic factors that cause a predisposition to marked pro-inflammatory pathways and immune system dysregulation
Whatever the cause, Lyme arthritis that continues to cause joint pain after antibiotics have been administered will require additional treatment to help sufferers manage their symptoms. Some of the most common treatments that may be attempted include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These are over-the-counter and prescription medications that both relieve arthritis pain and reduce inflammation. They’re usually taken orally, but they can also be applied to swollen joints as a topical treatment. The most well-known NSAIDs are aspirin, ibuprofen and Aleve.
- Anti-inflammatory medications: If your inflammation becomes extreme, your doctor may prescribe a potent and fast-acting anti-inflammatory medication to get this symptom under control. An example of this is corticosteroid medications.
- Prescription opioids: In rare cases, a patient may experience painful symptoms that are not aided by NSAIDs or other treatment options. In these instances, your doctor may prescribe opioids like codeine, hydrocodone or oxycodone. These are not recommended for long-term use, however.
If you would prefer to treat your arthritis symptoms naturally without medication, there are a few options you can try:
- Losing weight will put less pressure on joints, thus relieving pain.
- Low-impact exercises, like aerobics or swimming, allow for increased flexibility in your joints.
- Hot treatments for joint stiffness and cold treatments for pain, swelling and inflammation make a world of difference.
Your doctor may even recommend physical therapy to increase joint flexibility and muscle strength so that you can more effectively manage painful symptoms.
How Can You Prevent Lyme Disease?
The best way you can avoid Lyme disease in central PA, and indeed, anywhere there is a risk to human health, is to avoid walking in brushy, wooded areas with long grass. Other precautions you should take include:
- Tick-proof your yard. Clear leaves and brush on a regular basis and ensure you mow your lawn regularly.
- Cover up. When you’re in grassy or wooded areas, wear long pants tucked into your socks, shoes, a long-sleeved shirt, a hat and gloves. Wear light-colored clothing to make it easier to see ticks.
- Stay on trails. Try not to veer off from trails and avoid taking any routes through long grass or bushes. In addition, always keep your dog on a leash, as dogs are prone to tick bites, too.
- Wear insect repellent. An insect repellent with at least 20 percent or higher concentration of DEET will help protect your skin from tick bites. If you’re a parent of young children, you should always apply repellent to your kids rather than letting them do it themselves and take care to avoid their eyes, mouth and hands. Chemical repellents can be toxic, so always use them with care and be sure to read the label.
It’s also good practice to apply permethrin-containing products to your clothing for extra protection.
If you’re visiting anywhere that might have an active tick population, it’s important to be proactive about checking your family and pets for ticks. Deer ticks can be as small as a pinhead, so it’s imperative to be vigilant. Areas to particularly focus on checking are behind and in your ears, behind your knees, under your arms, on the back of your legs and anywhere else a small arachnid could escape detection. Also, the following precautions may help you find a tick before it’s too late:
- Check yourself, your children and your pets for ticks. After being out in any wooded area in Central PA, it’s a good idea to thoroughly check yourself, inside your belly button, under your arms, around your waist, in your body hair and hair on your head.
- Shower with a washcloth. It’s a good idea to shower as soon as you get home, as ticks can sit on your skin for hours before they bite, so showering with a washcloth can remove them before they have time to do any damage.
- Remove any ticks as soon as possible with tweezers. Either using regular tweezers or specialized tick tweezers that can be purchased from any outdoors store, you should quickly remove any ticks you discover on you, your children or pets. Gently grasp the insect near its head and pull steadily, and carefully, being sure not to crush or squeeze the tick. Once you have done this, dispose of the tick carefully and apply antiseptic to your skin.
- Never assume you’re immune. Even if you have had Lyme disease in the past, you can always get it again, so it’s crucial to remain aware of any risks in your area.
When it’s caught and treated as early as possible, Lyme disease can be fully treated, saving you from potential complications like arthritis and joint pain. You and your family can be tick aware while still enjoying the great outdoors and protecting your health.
If you have Lyme disease and you’re currently suffering from joint pain, contact us here at Orthopedic Institute of Pennsylvania (OIP) for an appointment.
OIP on the cutting edge of total joint replacements
The Orthopedic Institute of PA performed Total hip and knee replacements on patients of the Pennsylvania Employee Benefits Trust Fund (PEBTF) as part of a year-long trial in an attempt to improve outcomes and reduce costs. The results were published nationally by the Health Care Incentives Improvement Institute HCI3. The results can be summed up by HIC3’s comment: “what OIP pulled off is impressive.”
Patient satisfaction remained high, while costs were reduced by $4,189 per patient. Due to more effective pain management and advanced rehabilitation programs, hospital stays were shorter and more patients were discharged safely to the comfort of their own homes rather than to inpatient rehabilitation facilities.
HCI3 describes the excellent results as due to “the rather dramatic care process improvements achieved.”
Congratulations to our surgeons at The Orthopedic Institute of PA!
For additional information about the ‘The PEBTF Total Joint Bundled Payment Pilot: A Best Practices Summary’, check out HCI3’s Case Study online at: http://prometheusanalytics.net/sites/default/files/attachments/PEBTF-Case-Study_0.pdf



