Simply The Best 2021 Voting Now Open
Harrisburg Magazine’s ‘Simply the Best 2021’ voting is now open, and we’re asking for your help! We are honored to have been voted Simply The Best in the Harrisburg area for 10 consecutive years – Please help us make it 11!
If our team at OIP has helped you overcome injury or pain and get back to the things you enjoy most, please take a moment to vote for us in each of the four categories below.
Simply follow each link below and place your vote for OIP:
- Medical – Orthopedics (Click Here to Vote)
- Medical – Pain Specialist Clinic (Click Here to Vote)
- Health Services – Physical Therapist (Click Here to Vote)
- Local Favorites – Place to Work (101+ Employees) (Click Here to Vote)
We know that trust is earned, and respect your choice to choose your orthopedic provider – and when and where you have surgery. Thank you for choosing us!
OIP unveils new logo in its 50th year
Same Mission. Same Values. Same Physicians. A Brand New Look!
This year, we will celebrate our 50th year of service to Central Pennsylvania patients. Throughout the year we will be reflecting on our past, and more importantly, looking to the future of OIP as one of the region’s few remaining physician-owned and independent orthopedic groups. This year will bring several exciting announcements as we expand our presence and services to meet the needs of our community.
We are excited to share with you the first of these announcements…
Our NEW LOGO that represents both the history and future direction of the practice.
It reflects our mission to keep YOU, our patients, at the center of all we do. We strive to provide a complete circle of care to address all your orthopedic needs. From preventative services to immediate care. From conservative approaches to surgical interventions.
OIP Doctors Receive Education Awards
We congratulate Dr. DeLuca, Dr. Dahl, & Dr. Himmelwright for being recognized by UPMC Pinnacle for their ongoing contributions to teaching and education in the field of orthopedics. These doctors go the extra mile by offering their expertise to the next generation of doctors. Way to go!
Important OIP Family of Care Provider Update
To Our Family of Care Patients:
On May 23, 2020, the seven physicians in the OIP Arlington Division, (Timothy Ackerman, William Beutler, Matthew Espenshade, John Grandrimo, Scott King, Robert Maurer and Walter Peppelman) will no longer be a part of our OIP group practice. They will become employees of a hospital-owned group at UPMC Pinnacle.
If you wish to continue care with our OIP physicians, you do not need to do anything other than continue to make your appointments with us by calling 717-761-5530.
If you are planning to follow an Arlington Division physician to UPMC, please check your insurance plan as your co-pays and coverage could be affected.
You have the right of patient freedom of choice to select the physician as you wish, and OIP is prepared to serve you and meet your medical needs.
OIP gives $12,000 to Central Pennsylvania Food Bank
CAMP HILL, Pa. (PA), April 28, 2020- Orthopedic Institute of Pennsylvania’s charitable foundation donated $12,000 to Central Pennsylvania Food Bank in support of the food bank’s effort to distribute healthy, nutritious food to some of the most vulnerable in Central Pa. The donation will supply approximately 70,000 meals to thousands of households and individuals in Dauphin, Cumberland, York and Perry counties.

“What makes this special to OIP, is that we’re able to give back to the local communities that are at the heart of what we do,” said Will Thompson, CEO of Orthopedic Institute of Pennsylvania. “Through the Orthopedic Institute of PA Foundation Fund, of the Foundation for Enhancing Communities, we are able to reach outside our walls and tangibly help those in need.”
Thompson says “As we are here to serve our patients through this pandemic, we also understand the needs of our local community. Part of the mission of our foundation is to support those within our own backyard who may be facing difficulties.”
“We are so thankful to OIP for providing much-needed support to our Crisis Response,” said Joe Arthur, Executive Director of the Central Pennsylvania Food Bank. “The Central Pennsylvania Food Bank and its partner network have provided over 50% more food in the last month than in previous months and we believe demand will grow further as the economic crisis continues. Support like this also helps us provide the healthiest foods available.”
The Central Pennsylvania Food Bank welcomes this donation, and invites others to help bring food to needy families by making financial donations to the food bank. To make donations to help with the increased need in Central Pennsylvania communities during the COVID-19 Pandemic, visit www.centralpafoodbank.org. People in need of food assistance can call the Central Pennsylvania Food Bank’s helpline at 1-877-999-5964.
For orthopedic needs, OIP’s walk in clinic is open 7 days a week. Call 1-888-OUCH-OIP or click here for more information. OIP would like to encourage all those who are able to give to the Central Pennsylvania Food Bank to do so at this time.
Chronic Knee Pain: Causes and Treatments
Joint pain is bothersome in any form, but when it becomes chronic, it can be debilitating. Chronic knee pain can make the simplest tasks seem almost impossible. Everything from walking to sitting down can be painful, and coping with chronic knee pain without seeking treatment can make the situation even worse.
The knee joints are two of the strongest and most vulnerable joints in the body. Knowing what could injure them and how to properly treat any knee injury can be the difference between living an active life and living in discomfort.
What Causes Chronic Knee Pain?
The causes of chronic knee pain can vary, but they’re usually the result of two reasons:
- Trauma: Traumatic injuries are usually ones that happen suddenly, like falling. However, they can also be the result of repetitive motions or receiving a blow to the knee.
- Medical conditions: As we age, our bodies become more vulnerable to degenerative disorders, such as arthritis. Some of these conditions negatively affect the joints, leading to chronic pain.
Chronic knee pain causes ongoing discomfort in the knee — this can be in the form of swelling or sensitivity, and it can affect one or both knees. Traumatic injuries can lead to dislocation of the kneecap, a fracture or tears in ligaments or in the meniscus — which is a piece of cartilage that provides cushioning.
Traumatic injuries are often preventable with simple activities, like ensuring you warm up properly before exercising and using proper protective equipment when playing sports. Medical conditions aren’t always preventable, though.
Degenerative issues, like osteoarthritis or gout, or more serious concerns, like tumors, can result in chronic knee pain, and there’s little a person can do to prevent them. Other medical conditions that may lead to chronic knee pain include:
- Tendonitis: Typically a pain in the front part of the knee, tendonitis will only get worse with continued movement.
- Baker’s cyst: There is fluid in the knee that helps lubricate it, so it can bend easily and without pain. When this fluid builds up, it can form a baker’s cyst, which can cause ongoing knee pain.
- Bursitis: When the knee is overused, especially without proper rest, it can become inflamed, resulting in bursitis.
- Chondromalacia patella: Chondromalacia patella occurs when the cartilage below the kneecap has been damaged.
- Osteosarcoma: A type of bone cancer that most often happens in the knee, osteosarcoma is also the second most common type of bone cancer.
- Cellulitis: The good bacteria that live on our skin are meant to live on it, not in it. Cellulitis occurs when that bacteria ends up under the skin’s protective surface, causing a bacterial infection.
Chronic Versus Acute Pain
Pain is the body’s way of warning you, which is why it usually comes on quickly and eventually fades away. Pain from stubbing your toe or healing from surgery are both examples of acute pain, because they don’t last longer than a few months. In many cases, the pain will lessen and disappear as the cause disappears.
Alternatively, chronic pain doesn’t go away without medical intervention. However, chronic pain can also occur, even if the initial cause of pain heals or disappears because the pain signals remain active for a long time.
Usually, acute pain is fleeting and often goes away with time. Chronic pain, on the other hand, is the result of a singular significant incident and rarely goes away on its own — it requires diagnosing and treatment.
How to Diagnose Chronic Knee Pain
There are two steps to getting a chronic knee pain diagnosis: a consultation with a doctor, and any potential imaging or lab tests.
The doctor will determine which diagnostic lab tests are needed after they have performed a physical examination of your knee. They will ask you to bend the knee and may feel around to see if certain areas hurt more. Their conclusions will dictate which lab tests will be needed.
Lab or imaging tests for chronic knee pain diagnoses can include X-rays, blood work, MRIs or CT scans. You may need to go in for multiple imaging or lab tests, so the doctor can diagnose what type of chronic knee pain you have, so you can begin the appropriate treatment.
How to Treat Chronic Knee Pain
While chronic knee pain doesn’t fade away on its own, it is treatable. The type of chronic knee pain you’re experiencing will dictate which course of treatment is best for your situation.
There are several types of treatments that are options, including:
1. Therapy
Physical therapy helps strengthen the muscles around the painful area of the knee, which helps make it stable. Depending on the cause of your chronic knee pain, you may be prescribed physical therapy or just physical exercise to perform on your own at home.
If you’re active, the doctor may prescribe specific exercises that will help retrain how you use your knees to take some pressure off the injured one. Similarly, you may be required to wear a leg brace or invest in tools to improve your foot’s arch to redistribute your weight.
2. Injections
Your doctor may prescribe injections for chronic knee pain, which will help alleviate the pain for several months. Some substances that can potentially help include:
- Corticosteroids: This drug helps reduce the inflammation and symptoms of arthritis, leaving you pain-free for months. However, corticosteroids don’t work for everyone.
- Hyaluronic acid: This acid mimics the natural fluid used for lubrication in the knees. It increases mobility and reduces joint pain and can last for several months. However, the effectiveness of hyaluronic acid is contested.
- Platelet-rich plasma: Ideal for those whose chronic knee pain is due to ligament tears or sprains, platelet-rich plasma is a concoction of platelets from your own body to help heal injuries.
3. Medication
Pain-relief medication can sometimes be a simple answer to chronic knee pain. Your doctor may prescribe painkillers that are stronger than over-the-counter ones to help you manage any discomfort.
4. Surgery
Often used as a last resort, surgery is sometimes the most effective treatment for chronic pain. Surgery will likely only be an option after other treatments fail. When surgery does become an option, the type will be dependent on the specifics of your chronic knee pain.
One option is to try to fix whatever is injured, such as mending a torn ligament or damaged cartilage. Another option is to partially or completely replace the knee. Partial knee surgery replaces only the extremely damaged parts of the knee with artificial parts made of metal and plastic. A full knee replacement, as its name suggests, replaces the entire knee with an artificial joint.
Find Chronic Knee Pain Treatment Near You
There’s no need to suffer through chronic knee pain, especially when the Orthopedic Institute of Pennsylvania’s physicians are here to help. While surgery may end up being the best option, it is never the first one we suggest. We opt instead to work with each patient to find non-invasive ways to treat chronic pain.
With numerous locations across Pennsylvania, we’re dedicated to helping you live a pain-free life. To request an appointment at one of our locations, simply fill out the form online or call 717-761-5530.
Avoiding Re-Injuring Your ACL
In this article:
- What to Do After ACL Surgery
- What Not to do with a Torn ACL
- Recommended Activities for an ACL Injury
- How Do You know if You Tore your ACL After Surgery?
- Get ACL Help at OIP
The acute cruciate ligament (ACL) is a small but mighty part of the human body. Located in the knees, it connects the thigh bone to the shin bone, stabilizing the leg and allowing the shin bone to slide forward smoothly. Tearing this ligament can be both painful and debilitating, and ignoring the injury can lead to bigger problems down the line.
An ACL injury is most common among athletes — they also have a bigger chance of re-tearing their ACL, especially if they fail to follow rehabilitation guidelines, which begin as early as the day of the ACL surgery.
What to Do After ACL Surgery
Generally, ACL surgery is an outpatient procedure, which means you don’t have to stay in the hospital overnight. The surgery itself is fairly simple and uses a graft from the patient’s body to replace the torn ligament. General anesthesia is used and, once you’re awake, the medical staff will help you practice walking on crutches. You may also be fitted with a splint or knee brace.
You’ll be given instructions regarding cleaning and dressing your wound, which you should follow precisely. Failing to properly clean and dress the wound can lead to infection, which will only prolong healing.
The R.I.C.E. method is the most common recommendation to help the injury heal faster:
- Rest your leg and avoid putting any pressure on it.
- Ice the knee to help reduce swelling. Approximately 20 minutes of icing the knee ever two hours is recommended.
- Compression is another way to help the swelling go down. Wrap a compression wrap or an elastic bandage snugly around the knee.
- Elevation helps the blood flow away from the knee. Simply lie down with the injured knee propped up on a pillow.
The two goals immediately after surgery are to get any swelling to go down and ensure the wound heals quickly and properly. Avoid heating pads during this time, since heat will increase the swelling. Avoid putting any pressure on the injured leg until a doctor says you can.
Generally, you’ll be told to start putting slight pressure on the leg a few weeks after surgery. This is dependent on which type of ACL injury you had, such as a partial tear or a complete tear.
You’ll be expected to attend physical therapy to get the muscles around your knees stronger, so your knee can stabilize once again. If you’re an athlete, physical therapy will be crucial, but the timeline for when you can return to playing sports can vary greatly, especially since athletes tend to have a higher chance of re-tearing their ACL.
What Not to do with a Torn ACL
Tearing the ACL means your knee’s range of motion is limited. Physical therapy works to help you regain that range of motion, but it’s important to be patient and follow the physical therapist’s guide on what else not to do with your ACL injury. Doing too much too soon can result in a re-injury.
Physical therapy usually starts with gentle exercises to move the knee. As the wound heals, tougher exercises will be introduced. Because the ACL graft is still healing, it’s important to avoid stretching it. The physical therapist will show you ways to exercise the area without risking the ACL graft.
The goal of physical therapy is to help you begin to put pressure on the injured leg safely — this takes time and patience. It also requires you to abstain from activities that are risky for the ACL, such as running or swimming. Swimming can be beneficial, but it requires the muscles to work a bit harder against the pressure of the water. Tearing the ACL a second time is very possible if you return to swimming or running too soon.
Recommended Activities for an ACL Injury
From day one of your rehabilitation, you’ll be expected to begin exercising your injured leg. The best way to avoid re-tearing your ACL is to follow your physical therapist’s instructions. In the first few months, you’ll need to take it slow, working to strengthen the muscles around the ACL. Exercises such as riding a stationary bike and doing gentle leg presses are good for building up nearby muscles without straining the ACL.
If swimming is something you want to do, it’s best if you stick to activities that don’t require pumping your legs. Paddling with your arms is okay, but avoid paddling with the legs. The physical therapist will be able to tell you when you can begin swimming, based on the type of ACL injury you had and how your rehabilitation is coming along.
The full recovery time varies from person to person. However, studies have shown that those who wok on strengthening the muscles around the ACL and wait at least nine months before returning to sports are less likely to re-tear their ACL.
What to Do If You Re-Tear Your ACL
Knowing how to avoid re-tearing your ACL is important, but since the rate of re-injury is high, it’s beneficial to know what to do if you do re-tear it.
How Do You know if You Tore your ACL After Surgery?
To get an idea if you tore your ACL after surgery, you may hear a popping or cracking sound, which is usually followed by pain that is mild or severe. Swelling or tenderness is also common after an ACL injury, and there may be some redness around the knee.
If you’re unable to move or extend the knee, it’s a sure sign that there’s an injury. Contact your doctor right away and follow any instructions they give you.
The doctor will examine the knee and decide whether it’s an ACL re-tear or something else. If surgery is necessary, you will repeat the process from the initial ACL tear until the new injury heals.
Get ACL Help at OIP
The Orthopedic Institute of Pennsylvania exists to help you with any orthopedic injuries, whether they’re from playing sports or the result of an accident. With several locations across the state and walk-in clinics for orthopedic emergencies, we’re convenient and available to help.
Contact our walk-in injury clinic for 24/7 emergency advice by calling 855-OUCH-OIP or request an appointment by calling the main line at 717-761-5530.
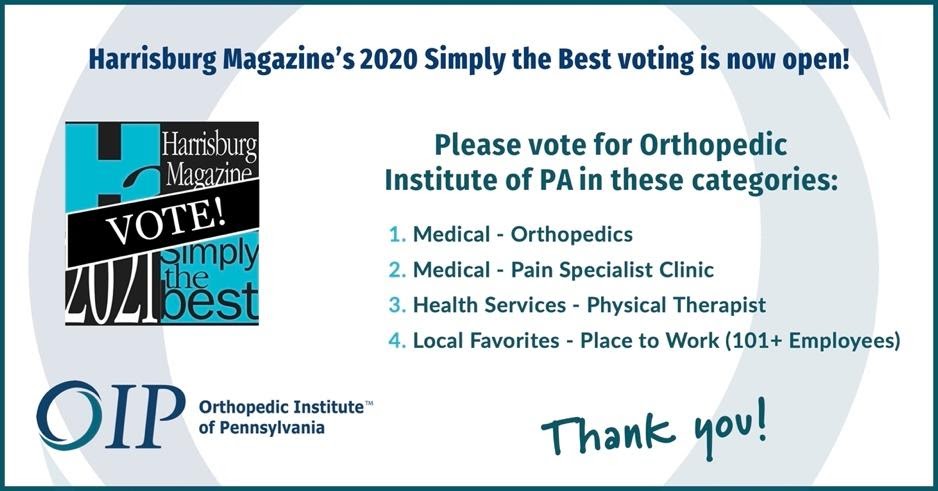
Simply The Best 2020 -Vote for us!
Harrisburg Magazine’s Smply the Best 2020 voting is now open. Please vote for us in all categories for all locations shown in the photo. Follow this link to cast your votes: https://
Thank you!
Tips for Finding a Job in the Medical Field as a New Graduate

Medical careers are among the fastest-growing occupations in the U.S. Demand for home health aides, personal care aides and physician assistants is expected to grow over 30% by 2028. There’s also a great demand for nurse practitioners, phlebotomists, physical therapist aides and medical assistants, among many others.
If you recently graduated from a medical program, you’re likely excited to get started on your new career. Although the medical field is a fast-growing industry, it can be competitive for new grads. With some business know-how, preparation and determination, you can find the right fit for you and your goals.
How to Get a Job in the Medical Field
Searching for your first medical job will, in itself, feel like a full-time job. However, if you’re prepared, organized, patient and ready to tackle challenges, you’ll land the job you’ve been hoping for. The key is not to get discouraged along the way. Here’s what you can do to increase your chances of finding a job that’s a good match for your skillset and education.
1. Network

Networking presents numerous opportunities and can be a great way to launch your career. When you connect with others in your field, you might learn of a job opening before it’s ever posted. Up to 85% of jobs are found through networking. At least 70% of jobs are never advertised.
As a graduate of a medical program, aim to build relationships with peers, people who work in your field and recruiters. One way medical professionals can network is to join a professional organization. For example, a recent grad of a medical assistant program might become a member of the American Association of Medical Assistants (AAMA) and attend conferences, programs and events. Most health care careers have an association or society you can join.
2. Tailor Your Resume and Cover Letter
Make sure you have a solid resume to highlight your skills and show how you’ll be an asset to a potential employer. Research relevant job descriptions and highlight key skills in your resume. For example, medical career recruiters might look for candidates with excellent attention to detail or strong interpersonal skills.
You don’t need to rewrite your entire resume for every position you apply to, but you will want to edit a few lines to ensure it fits a specific employer’s needs. Make sure your resume also includes the following elements:
- Statement of career goals that relate to the position.
- Academic accomplishments.
- Career experiences.
- Related activities such as internships or volunteer work.
It’s important to submit a cover letter with each resume and job application to express your enthusiasm and showcase your unique background. Here are tips for creating an impactful cover letter:
- Keep the cover letter short, or no longer than a few paragraphs on a single page.
- Use the cover letter to highlight your strengths and how they relate to the specific opening.
- Show you researched the company, and you’re excited about the position.
- Customize the letter for the company and the job.
Consider sharing your resume and cover letter with the career center at your school to receive valuable feedback. There are also plenty of templates and resources online to help you construct a professional-quality resume for free or at a low cost.
3. Search Every Day
There’s no doubt about it – health care jobs are in demand. However, it’s also a competitive market, and a single employer might receive thousands of applications a year. For this reason, it helps to treat your search like a full-time job and look for opportunities every day. A few online resources for medical job seekers include:
Other general job search sites that are considered among the best include:
- Indeed
- CareerBuilder
- SimplyHired
- Monster
- Glassdoor
You can also search employers’ websites and job boards of professional organizations in your desired field. Apply to as many openings as you can, but avoid wasting time with jobs you wouldn’t take. Remember to check out other resources like job fairs, temporary agencies and newspapers.
4. Follow Up
Don’t wait to hear back. Aim to follow up with companies you’ve applied to a week later. When you reach out to a potential employer after applying, you put your name to the front of their mind and help yourself stand out from the dozens of other candidates. Contact the hiring manager by email or phone and briefly restate your interest in the position and why you’d be a good match.
5. Be Flexible
If you struggle to find a position in your field right after graduation, consider volunteering or taking an internship at a local hospital or medical facility, even if it’s a non-medical role. This will help you network, gain experience and land a job when one opens up. You might also consider looking for work outside of your major or in a different location.
6. Prepare for the Interview
The interview is one of the most critical aspects of your job search. It’s your chance to show a potential employer how you can meet their needs. It’s also the time to ask questions and determine if the company is right for you. The key to making a lasting impression is to properly prepare. Here are tips to help you enjoy a successful interview:
- Research the employer and the job opening.
- Prepare thoughtful answers to common interview questions and practice.
- Compile a list of questions to ask the employer.
- Bring copies of your resume and a list of references.
- Dress appropriately.
- Bring a notepad to jot down information.
- Show your enthusiasm, focus on the positive and respond honestly.
- Plan to arrive ten minutes early.
Reach Out to Orthopedic Institute of Pennsylvania
The Orthopedic Institute of Pennsylvania (OIP) understands that the ability to help patients live healthy pain-free lives makes a medical career worth it every step of the way. If you live in central Pennsylvania and are interested in joining a team of dedicated and empathetic professionals, we invite you to browse our open positions. To connect with a team member and learn more about our mission and services, contact us today.
Decrease Pain and Recovery Time of Knee Joint Replacements With Mako Robot
Depending on where your arthritis is affecting your knee, a surgeon may recommend either a partial knee replacement or a total knee replacement. With both procedures, the surgeon replaces the damaged or diseased joint with an artificial implant to restore function and relieve pain.
Stryker, a medical technology company based out of Kalamazoo, Michigan, has developed technology called the Mako robot, which assists surgeons in performing knee replacements. It can help decrease a patient’s pain, recovery time, soft tissue damage and bone damage resulting from the procedure.
The Mako robot application got the approval of the Food and Drug Administration in 2015. However, Stryker officially announced the launch on the first day of the 2017 annual American Academy of Orthopedics Surgeons meeting in San Diego. Today, the Orthopedic Institute of Pennsylvania is using this exciting robotic-arm assisted technology for knee replacement surgeries.
About Knee Replacement
Knee replacement surgeries originated in 1968. When walking assistants and medications no longer provide relief or help to restore mobility and function, you might want to consider a knee replacement surgery. Depending on how severe your arthritis is, your surgeon may recommend partial or total knee surgery:
- Partial knee replacements are surgical procedures that help ease arthritis in one or more of the three knee compartments: the medial (inside) component, the lateral (outside) component or patellofemoral (top) component. In this procedure, the surgeon only replaces the damaged knee joint area, helping to reduce trauma to healthy tissue and bone.
- Total knee replacements are surgical procedures where the surgeon replaces the entire injured or diseased knee.
About Mako Robot System Features
Mako robot technology offers an individualized surgical plan based on your own personal anatomy. In both partial and total knee replacement procedures, the orthopedic surgeon guides the Mako robotic arm to eliminate diseased cartilage and bone. The Mako robot system:
- Uses full flexion and extension, enabling the pre-resection capture of kinematic tracking specific to the patient.
- Plans implant size, alignment and orientation accurately, using CT-derived 3D modeling.
- Promotes bone-sparing and minimal tissue trauma.
- Provides a faster recovery, due to its minimally invasive procedure.
- Offers proper soft tissue balance and correct knee kinematics from real-time intra-operative adjustments.
The Mako robot is the most consistently accurate joint replacement technology available worldwide today. It allows surgeons to optimize knee implant sizing, ligament balance, and implant longevity and function. It’s an innovative procedure option for individuals who live with mid-stage osteoarthritis in the patellofemoral, medial or lateral knee compartments.
Overview of Mako Total Knee Replacement Procedure
With Mako technology, you can have an individualized plan for your knee replacement surgery. First, the doctor will take a CT scan of your knee joint. They’ll upload the CT scan into the Mako system software, which will create a 3D knee model. The doctor then uses the model to pre-plan and help your surgeon perform your knee replacement.
The surgeon will follow your individualized plan while they prepare the bone for the knee implant. The surgeon will then guide the robot arm to eliminate any diseased cartilage and bone. The Mako technology helps the surgeon stay within the boundaries of the predefined area, so no other bone or tissue is affected.
Following your surgery, the surgeons, physical therapists, doctors and nurses will help you set goals so you can get back to regular movement in your knee and surrounding areas. They’ll monitor your condition and recovery progress closely. Your surgeon might take an x-ray of your new knee replacement to review it with you.
Benefits of Knee Joint Replacements With Mako Robot
Knee replacements help people get back to their lives. They can improve a patient’s mobility, pain levels and quality of life. Moreover, knee replacements using the Mako robot have several additional advantages. Besides offering increased precision, some benefits of Mako knee replacements include:
Reduced Soft Tissue and Bone Damage
One study, published in The Journal of Arthroplasty, compared the results of 30 consecutive manual total knee arthroplasty surgeries, or TKAs, and 30 consecutive Mako TKA surgeries — all performed by the same surgeon. The results showed that the patients who had the Mako-assisted procedures had less bone and periarticular soft tissue injury than the patients who had the manual TKA surgeries.
Decreased Pain
It’s common for individuals to try conservative treatments and medication to treat their knee pain. However, if you’ve tried these approaches and aren’t experiencing adequate relief, you might be an ideal candidate for Mako knee replacement, which could offer you relief.
If you’re experiencing start-up knee stiffness and pain when you move from a sitting position, a Mako surgery might be able to help. Joint degeneration and arthritis pain can:
- Come and go.
- Be constant.
- Occur after a rest period.
- Occur with movement.
- Be located in many parts of your body.
- Be located in one particular part of your body.
In one clinical study, those who underwent Mako partial knee replacement felt less pain in their 90-day postoperative period. The study’s results showed those who underwent robotic arm-assisted surgery reported substantially lower levels of postoperative pain. There was also a 55.4% lower median pain score in the robotic-arm assist group, compared to manual patients from the first day of the study to the eighth week.
Shorter Recovery Time
The Mako surgery’s minimally invasive nature allows you to:
- Walk shortly after.
- Return to regular day-to-day activities sooner.
- Drive a vehicle within your first few weeks.
Mako helps with recovery from knee joint replacement and spares your healthy tissue and natural bone. It helps to preserve as much of your knee as possible, unlike more invasive surgeries. The robotic arm helps to optimally position the knee implant, making your knee feel more natural after the procedure. Other types of total knee replacement procedures require a longer hospital stay and recovery, but the robotic arm used in a Mako surgery offers pinpoint accuracy, which promotes a shorter recovery time.
Contact the Orthopedic Institute of Pennsylvania for Your Mako Knee Joint Replacement Surgery
The Orthopedic Institute of Pennsylvaniapledges to provide compassionate and caring service to make sure each and every patient has a positive experience. We’re dedicated to placing your needs first. We’re committed to meeting and going beyond each patient’s expectations to offer outstanding and exceptional care.
Contact our office today to make an appointment for your Mako knee joint replacement consultation.