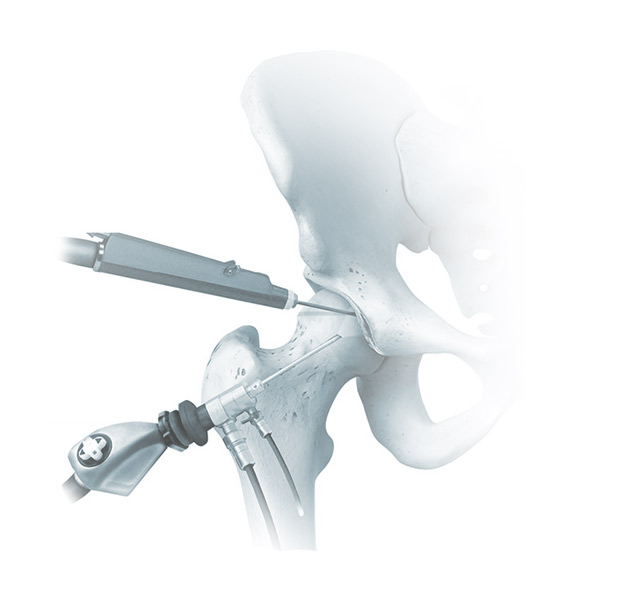
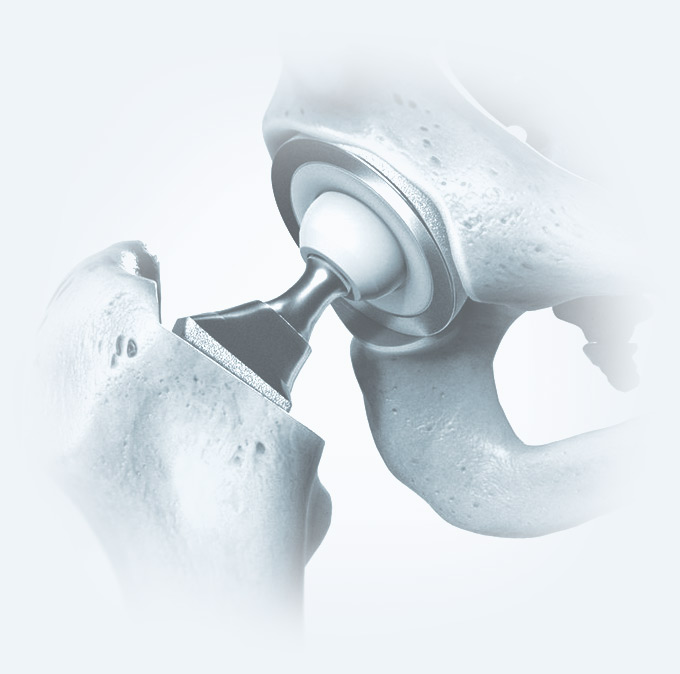
Advanced Treatment Options for Hip Issues
At OIP, we provide a wide range of advanced treatment options for hip pain and injuries, tailored to your individual needs. Whether you’re suffering from arthritis, bursitis, or another hip condition, our experienced orthopedic specialists are here to help. Explore the treatment options below, including real stories from our patients who have experienced life-changing results.
4.9 stars 4.95 out of 5 (1611 reviews) About star rating